
August • 28 • 2024
Ambulatory Care Exposures Result in High Claims Frequency and Severity
Summary
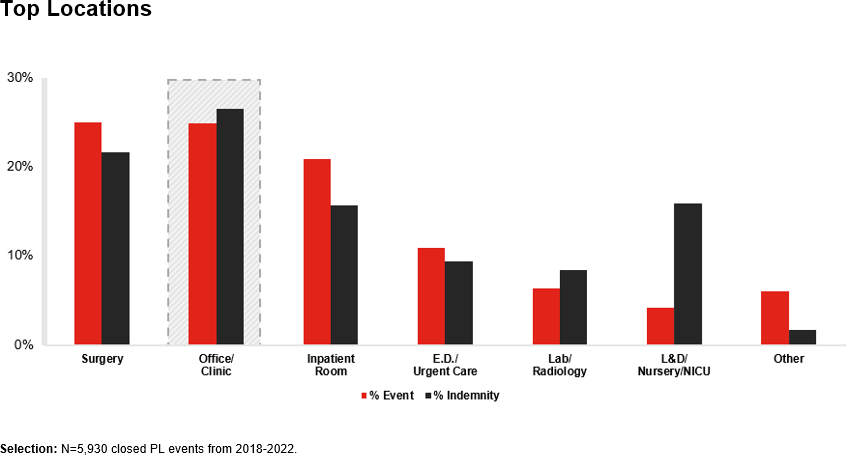
Claims data shows that ambulatory care settings are associated with frequent and costly medical malpractice claims.
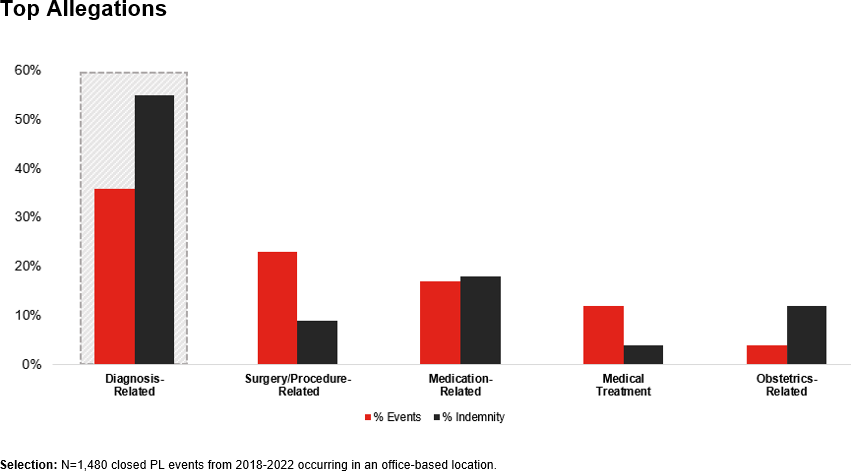
Diagnosis-Related Events Are the Most Frequent and Costly
Further analysis revealed that diagnosis-related allegations accounted for 36% of claims and 55% of indemnity paid. (Surgery came in second at 23% of events and 9% of indemnity paid.) This finding is not unique to the office setting as diagnosis-related claims are the most common allegation in medical malpractice claims in most settings.
General Medicine Accounts for the Largest Share of Claims
Although malpractice claims may occur in any specialty, general medicine accounted for the greatest share of both claims frequency (31%) and indemnity paid (45%).
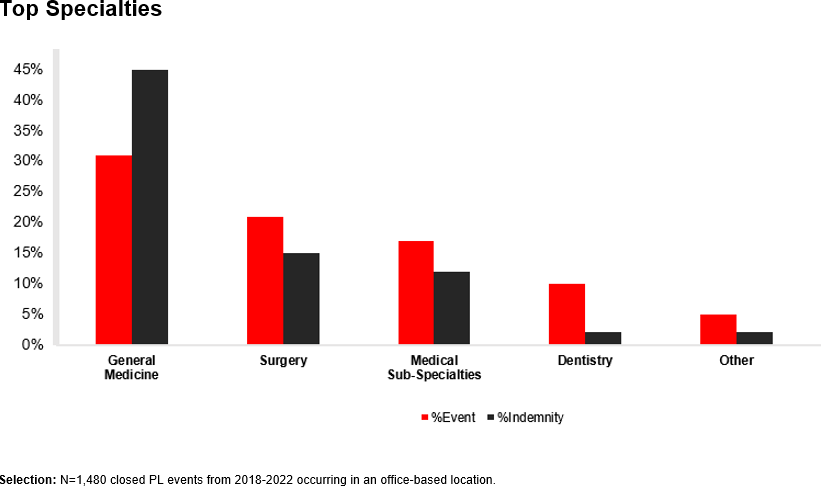
Some medical subspecialities experienced higher rates of claims than others. For example, pain management saw 53 claims and 29% of indemnity, whereas dermatology had 51 claims and 12% of indemnity. In comparison, addiction medicine had just one claim and 0% of indemnity.
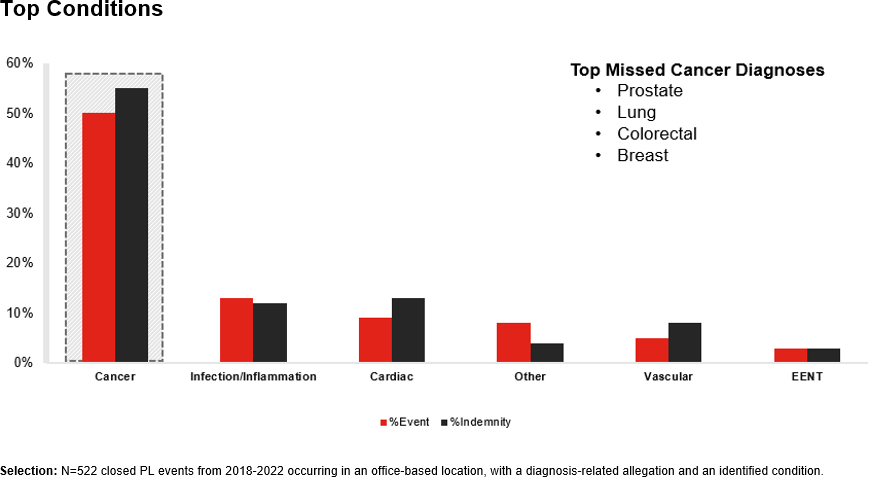
Cancer Is the Most Common Type of Diagnosis-Related Claim
Diagnosis-related claims tend to be severe – with 55% resulting in death or high-severity injury. Missed or delayed cancer diagnoses were the most common type of diagnosis-related claim. The top missed cancer diagnoses were prostate, lung, colorectal, and breast cancer.
Key Risk Management Issues
Following are the top three risk management issues that emerged from our claims data analysis:
- 36% of claims involved clinical decision-making issues. The diagnostic process involves multiple steps, some of which are driven by data and others of which are rooted in intuition. This leaves plenty of opportunities for errors. Some claims stem from a narrow diagnostic focus that may be influenced by cognitive biases. Other times, providers may fail to order the appropriate tests or fail to obtain a needed consult or referral. In other instances, an adequate family or personal history, especially a history of cancer, may not be obtained. All these things alone, or in combination, can result in a missed or delayed diagnosis.
- 15% of claims involved clinical system issues. In many cases, errors stem from issues in the system rather than the actions of an individual provider. System issues involve oversights such as failure to manage follow-up care, failure to screen, or the mismanagement of test results, resulting in providers being unaware of the results.
- 10% of claims involved behavior-related issues. Behavior-related issues often involve a lack of patient engagement that eventually leads to adherence issues. Determining why patients choose not to follow treatment recommendations is more complex, but problems often develop over time and may be due to a lack of education, poor engagement, unrealistic expectations, or social or cultural barriers.
How to Prevent Claims in the Office Setting
Understanding the top risk management issues can help healthcare leaders take steps to reduce exposures and set their providers up for success. Following are risk recommendations to help address these top issues.
Clinical decision-making. Training helps providers become aware of their own cognitive biases, whereas clinical decision support tools help providers avoid missed diagnoses. Other steps include:
- Developing a medical history and physician examination (H&P) policy that includes documentation of specific elements that providers update every visit.
- Ensuring patient information is complete and centralized.
- Implementing a quality review process for follow-up on test results and diagnostic accuracy.
- Following evidence-based preventative health screening guidelines and documenting completed informed refusal or deferment of preventive testing since missed cancer diagnoses are common.
Clinical systems. Since failures in clinical systems often relate to test results, tracking, and referrals, policies that address these issues prevent claims. Key steps include refining processes for follow up on test results, particularly critical results and incidental findings. Consistent documentation; clear, effective communication; and good EHR practices also help reduce failures.
Communication. Establishing clear expectations up front can improve patient engagement and understanding of treatment recommendations. This may involve providing clear instructions and ensuring patients understand their rights and responsibilities. Providers should work to understand the patient’s goals and identify barriers to care before these become a problem. Communication skills also play a role – the most effective tone is kind and positive. If conflict occurs, an honest and compassionate conversation, along with the implementation of behavioral agreements or contracts, may resolve the issue.
Taking these additional steps can help ambulatory care providers reduce the incidence of claims while also improving patient outcomes.
This article is based in part on “Ambulatory Care: Using Claims Data to Mitigate Risk,” presented by Heidi McCoy, MSN, BSN, RN, CPHRM, CPPS, and Marlene Icenhower, BSN, JD, CPHRM.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.