
View Expert Insights
October • 22 • 2025
Strengthening Care Delivery With Failure Mode and Effects Analysis
Article
Summary
Uncover process vulnerabilities, prioritize risks, and implement targeted improvements—leading to safer, more consistent patient care.
Do you know where your care delivery is most likely to fail? A failure mode and effects analysis (FMEA), along with a root cause analysis (RCA), will help you identify potential weaknesses in patient care processes, ultimately leading to better, more consistent care, and the avoidance of incidents that could harm patients and lead to liability.
The FMEA explores three key aspects of potential failure:
It can be helpful to perform an FMEA when developing new processes or service delivery procedures. By conducting the analysis early in development, you’ll identify and eliminate related concerns. You can also use an FMEA on existing processes to identify potential failures and redesign processes to reduce the possibility of failure.
When conducting an FMEA, it’s important to follow a methodical, step-by-step process.
1. Select a process to evaluate. The Institute for Healthcare Improvement (IHI) recommends focusing on a process that does not involve too many sub-processes. If you are trying to evaluate a large and complex process, break it into smaller parts.
2. Recruit a multidisciplinary team. Include everyone who is involved in the process at any point. If they are only involved in a small part of the process, they do not need to participate in the entire evaluation. Instead, bring them in specifically for the relevant discussions.
3. Have the team list all the steps in the process you are evaluating, in order. Include every step, even if it seems minor.
4. List the failure modes, failure causes, and failure effects for each step. Be thorough.
5. For each potential failure, assign a risk priority number (RPN). Calculate the RPN by multiplying:
6. Evaluate the results. Once you’ve identified the failures and assigned an RPN, you’ll be able to prioritize the potential failures that require your attention first.
7. Use the RPNs to plan improvement efforts. Once the FMEA is complete, create a plan to reduce harm from the failures you’ve identified. You can also use the FMEA to assess the potential impact of planned changes and to monitor and track improvement over time.
An RCA is different from an FMEA in that it identifies the underlying factors in performance variances, including those that may lead to sentinel events. It focuses on the systems and processes rather than individual performance and is non-punitive. As such, this analysis is not appropriate for events such as criminal acts, patient abuse, substance use, or intentionally unsafe acts.
To conduct an RCA, follow this step-by-step process:
The 5 Whys process is a simple RCA method first developed by Toyota. The idea is that you ask “why?” five times to drill deeper into the root cause of an issue. For example:
By utilizing FMEA and RCA processes, the healthcare team can find and correct flaws to improve patient care.
This article is based, in part, on “FMEA & RCA” – a presentation by Paul Frigoli, PhD, RN, BSN, CPHRM, CPHQ, MBB.
Failure Mode and Effects Analysis
The FMEA explores three key aspects of potential failure:
- Failure modes: What could go wrong?
- Failure causes: Why would the failure occur?
- Failure effects: What are the potential consequences of each failure?
It can be helpful to perform an FMEA when developing new processes or service delivery procedures. By conducting the analysis early in development, you’ll identify and eliminate related concerns. You can also use an FMEA on existing processes to identify potential failures and redesign processes to reduce the possibility of failure.
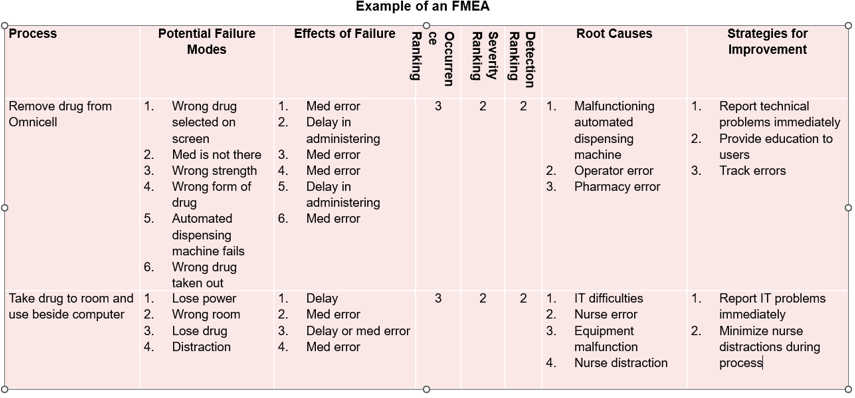
How to Conduct an FMEA
When conducting an FMEA, it’s important to follow a methodical, step-by-step process.
1. Select a process to evaluate. The Institute for Healthcare Improvement (IHI) recommends focusing on a process that does not involve too many sub-processes. If you are trying to evaluate a large and complex process, break it into smaller parts.
2. Recruit a multidisciplinary team. Include everyone who is involved in the process at any point. If they are only involved in a small part of the process, they do not need to participate in the entire evaluation. Instead, bring them in specifically for the relevant discussions.
3. Have the team list all the steps in the process you are evaluating, in order. Include every step, even if it seems minor.
4. List the failure modes, failure causes, and failure effects for each step. Be thorough.
5. For each potential failure, assign a risk priority number (RPN). Calculate the RPN by multiplying:
- The likelihood of occurrence (how likely the failure is on a scale of 1 to 10, with 10 being the most likely).
- The likelihood of detection (how likely you are to detect the failure, on a scale of 1 to 10, with 10 being the LEAST likely to be detected).
- The severity (how likely the failure is to cause harm, on a scale of 1 to 10, with 10 being the most severe).
6. Evaluate the results. Once you’ve identified the failures and assigned an RPN, you’ll be able to prioritize the potential failures that require your attention first.
7. Use the RPNs to plan improvement efforts. Once the FMEA is complete, create a plan to reduce harm from the failures you’ve identified. You can also use the FMEA to assess the potential impact of planned changes and to monitor and track improvement over time.
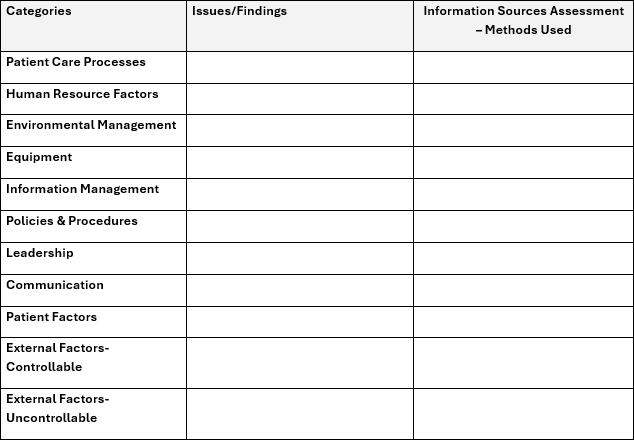
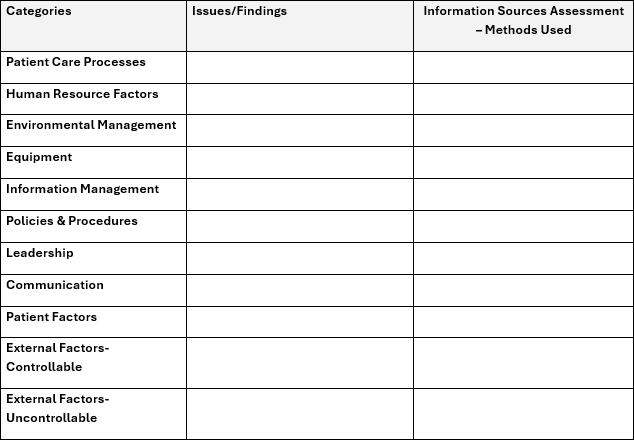
Root Cause Analysis
An RCA is different from an FMEA in that it identifies the underlying factors in performance variances, including those that may lead to sentinel events. It focuses on the systems and processes rather than individual performance and is non-punitive. As such, this analysis is not appropriate for events such as criminal acts, patient abuse, substance use, or intentionally unsafe acts.
- You can also use an RCA to identify serious adverse events – events identified from incident reports, near misses, medication errors, customer complaints, employee concerns, and facility incidents. The goal is to create an action plan that identifies strategies to reduce the risk of similar events occurring in the future. To do this, it’s necessary to identify active errors that occur between humans and complex systems, and latent errors that occur within healthcare systems.
Conducting an RCA: The 5 Whys
To conduct an RCA, follow this step-by-step process:
- Gather the facts using a timeline and interviews.
- Understand what happened.
- Identify the root causes.
- Develop a risk reduction plan.
- Evaluate the effectiveness of the actions taken.
The 5 Whys process is a simple RCA method first developed by Toyota. The idea is that you ask “why?” five times to drill deeper into the root cause of an issue. For example:
- Why is the patient’s intravenous run rate wrong? Answer: The previous nurse didn’t change the run rate.
- Why didn’t the previous nurse change the run rate? Answer: The doctor’s order had gone to the pharmacy, and the medication administration record (MAR) was not updated.
- Why wasn’t the MAR updated? Answer: The MAR is updated only once a day.
- Why is the MAR updated only once a day? Answer: The hospital has chosen to use oral instructions for more frequent updates.
- Why does the hospital use oral instructions? Answer: The process was created a decade ago, when medication orders changed less frequently due to longer lengths of stay.
By utilizing FMEA and RCA processes, the healthcare team can find and correct flaws to improve patient care.
This article is based, in part, on “FMEA & RCA” – a presentation by Paul Frigoli, PhD, RN, BSN, CPHRM, CPHQ, MBB.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.