
View Expert Insights
June • 13 • 2025
The Connection Between Physician Health and Patient Safety
Article
Summary
Research has found a link between physician health and malpractice claims. Providing resources to support healthcare providers is therefore important for both physician wellness and patient outcomes.
Physician Burnout and the Impact on Patient Safety
A landmark study observed an important connection between physician health and malpractice claims. Titled Physician Health Programmes and Malpractice Claims: Reducing Risk Through Monitoring, it considered whether physician health programs had an impact on malpractice claims. Data from 818 clients revealed a 20% lower malpractice risk among physicians enrolled in the program compared to physicians who were not enrolled.
A physician health program provides support to physicians who are struggling with addiction, physical, and/or mental health challenges. The study demonstrated that such programs are critical for both physicians and the patients they treat. Since then, the issue has become even more important considering the high levels of physicians experiencing burnout.
The Challenges of Physician Burnout
According to the American Medical Association (AMA), 53% of physicians reported experiencing at least one symptom of burnout. In 2023, a slight improvement was noted, dropping to 48.2%. While this is slightly encouraging, burnout is still a problem, with some groups being more impacted than others:
- Gender: 54.5% of female physicians report burnout symptoms, compared to 42.0% of male physicians. Female physicians were also less likely to feel valued.
- Specialty: The highest burnout levels were in emergency medicine, where 56.5% of physicians reported symptoms. Other specialties with high levels of burnout included internal medicine, obstetrics and gynecology, family medicine, pediatrics, and hospital medicine.
- Length of time in practice: Physicians who had been practicing for six to 10 years reported the highest levels of burnout (at 61.0%), while physicians who had been practicing for 20 years or more reported the lowest levels of burnout (at 41.3%).
A recent study published in JAMA Psychiatry, National Incidence of Physician Suicide and Associated Features, found that female physicians have a significantly higher suicide rate compared to the female general population. This is not true among male doctors – in fact, male physicians have a lower suicide rate than the general male population.
Physician burnout, as well as coexisting issues with substance use and physical/mental health matters, may also have a direct impact on patient care.
Claims Data and the Physician Health Connection
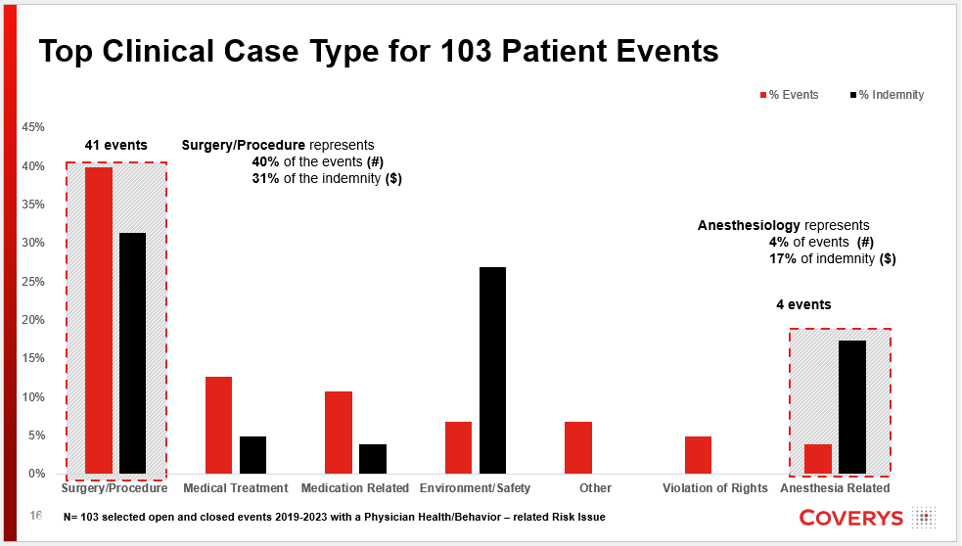
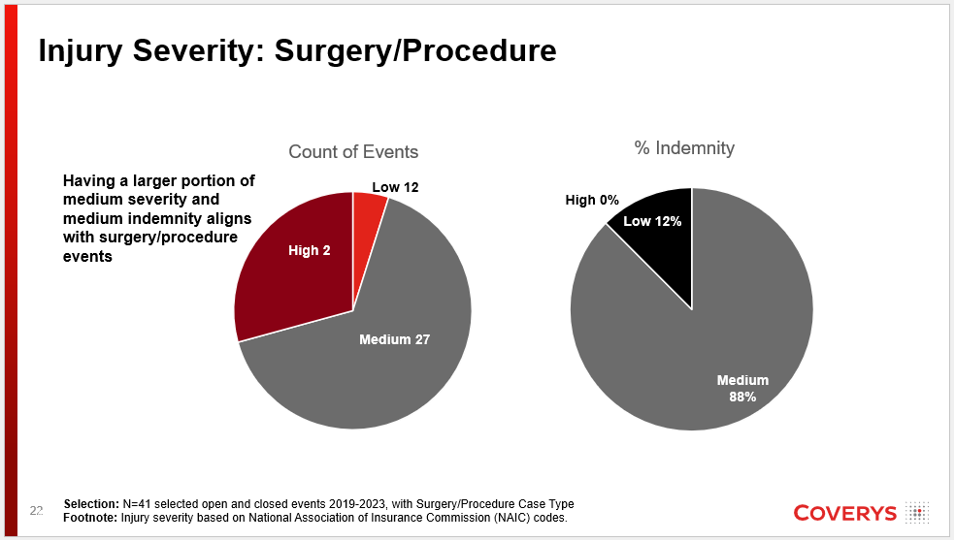
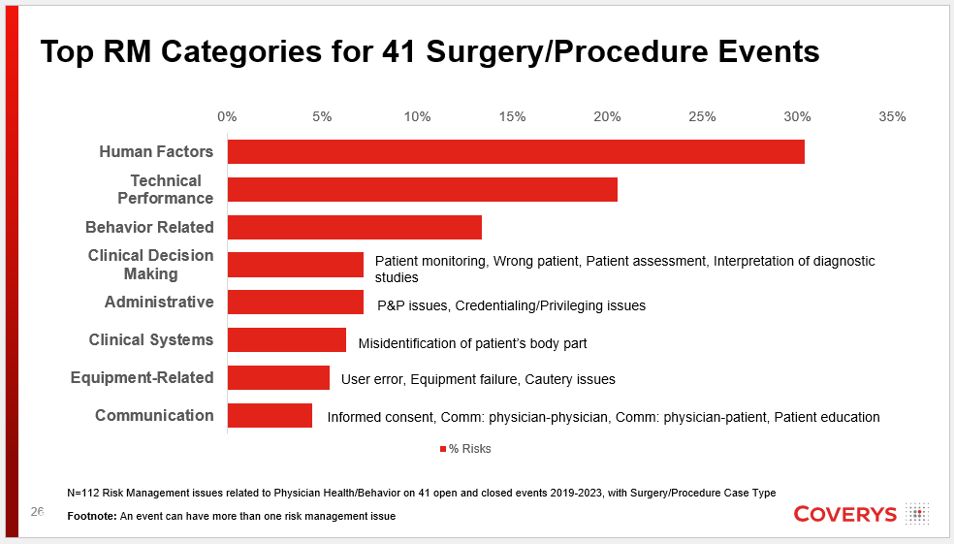
To further explore the link between physician health and patient safety, Coverys conducted an analysis of 6,050 medical professional liability events between 2019 and 2023. Risk management issues associated with physician health and behavior were used to select a target data set of 103 events. An event represents the entire patient clinical experience. The risk management issues included in the analysis were:
- Provider/staff behavior
- Distractions/lack of situational awareness
- Fatigue
- Alarm fatigue
- Ethical issues
Notable Claim
While aggregate data informs risk mitigation strategies, it is the individual stories that best highlight the importance of physician health. In one notable claim, a patient who underwent a colonoscopy asked the anesthesiologist if the doctor was drunk before the procedure began. The anesthesiologist reassured the patient everything was fine, and the procedure proceeded. Sometime during the procedure, the anesthesiologist detected the smell of alcohol and filed a report once the procedure was completed. The doctor failed a breathalyzer test, and the patient needed a repeat procedure, which resulted in the identification of concerning polyps that were missed in the first procedure.
Other patient events involving substance use, poor decision-making, or cognitive decline resulted in worse patient outcomes (including patient death) and large indemnity payments.
Supporting Physicians and Developing a Culture of Safety
According to the CDC, a culture of safety leads to a decrease in adverse events, improves quality of care, and increases patient satisfaction. Healthcare workers also benefit from a culture of safety, as it is associated with fewer healthcare injuries.
A commitment to a culture of safety includes:
- Recognizing and reporting high-risk exposures
- Developing and implementing prevention and control standards, policies, and strategies
- Providing resources that address safety concerns
It’s important to ensure all members of the healthcare team feel comfortable reporting their concerns. If they are afraid to report issues out of fear of punishment, problems may go uncorrected until an adverse event occurs. Research published in the AMA Journal of Ethics states that under a just culture perspective, punishment should be reserved only for those who have willfully and irremediably caused harm.
Research also highlights the importance of prompt recognition and follow up when physicians demonstrate objective indicators that may indicate they are not fit for duty. Colleagues, administrators, and other individuals “should record details of aberrant behaviors, performance deficiencies, and psychosocial problems” as red flags warranting compassionate follow up before a patient safety event occurs.
How Support Makes a Difference
A supportive approach is crucial. The following fictitious example illustrates a compassionate reaction that incorporates individual support, timely response to objective indicators that may indicate one is unfit for duty, and review of systems that may be contributing to physician burnout.
- Scenario: A physician was struggling with a heavy workload that required additional hours at home, while also dealing with personal stressors. She felt isolated, overwhelmed, and had lost her joy for work.
- Burnout identification: A medical assistant noticed that the physician seemed fatigued and distracted. The assistant asked the physician how she was doing, and she said she was fine. Shortly after, the medical assistant noticed the physician charting in the wrong patient’s record. She decided to share her concerns with the practice administrator.
- Response: The practice administrator spoke to the physician in a compassionate and supportive manner and referred her to the state physician health program (PHP). The physician received treatment and monitoring before she returned to work. Meanwhile, the administrator examined scheduling practices to reduce the workload for physicians.
Despite some recent headway, physician burnout remains an ongoing problem – and it’s a challenge that must be taken seriously. Creating psychological safety to allow all members of the healthcare team to report concerns and responding to those concerns in a compassionate manner will embed a culture of safety within the organization and help mitigate associated risk.
This article is based, in part, on a Coverys presentation “Clinical Claims Data Analysis: Patient Safety and Physician Health” by Susan L. Montminy, EdD, MPA, BSN, RN, FASHRM, CPHRM, CPPS.
Copyrighted. No legal or medical advice intended. This post includes general risk management guidelines. Such materials are for informational purposes only and may not reflect the most current legal or medical developments. These informational materials are not intended, and must not be taken, as legal or medical advice on any particular set of facts or circumstances.